Alternatives To Testing Sterility In Cell- And Tissue-Based Products
A conversation with Anthony Thatcher and Prethib Arumugam, Sumitomo Pharma America
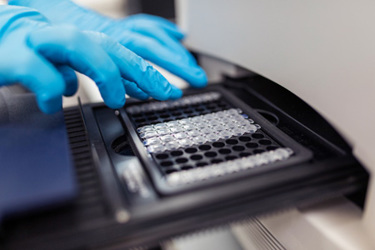
Inherent product variability, small sample sizes, and a greater amount of manual handling to produce cell- and tissue-based products make sterility testing especially challenging.
As the demand grows for faster release of these products, alternative testing methods are emerging, which, in turn, leads to a new set of challenges since any new assays must be validated and accepted by regulators.
The balance between sterility assurance and maintaining the product’s viability and function is a constant concern, as over-testing can deplete limited and expensive drug product. Regulatory agencies, including the FDA and EMA, are increasingly supportive of alternative methods, provided they are backed by robust validation data.
Anthony Thatcher, senior director of manufacturing operations for Sumitomo Pharma America, and Prethib Arumugam, associate director of quality control, earlier this month at the International Society for Pharmaceutical Engineering’s 2025 ISPE Aseptic Conference in Washington, D.C. We asked for a summary of their talk and had a few specific questions. Here’s what they told us.
Why is sterility especially challenging for cell- and tissue-based products compared to other aseptically produced therapies? How does the product influence test method selection?
Sterility testing for cell- and tissue-based products is inherently more challenging than for traditional aseptically produced therapies due to several key factors. The main issues are limited sample availability due to overall limited product availability, short shelf life relative to time taken to complete testing, higher risk of contamination due to manual and complex processing, and complex sample matrices containing materials that could interfere with detection.
Some of the factors to consider when selecting a test method for a product are the speed needed to release the product for patient administration, presence of cell or cellular debris in the sample, presence of any antimicrobial agents that require neutralization, and so on.
Can you describe alternative test methods? What are the benefits or drawbacks when it comes to sensitivity?
Any alternative sterility test methods must be demonstrated to be comparable to the compendial sterility testing methods. This often presents a challenge for new testing technologies as speed of detection often comes with limited sensitivity in terms of detecting a wide range of contaminants or detecting contaminants at low concentrations. However, even if these alternatives might be deficient as a direct replacement for compendial sterility testing, they might be valuable and suitable as supplemental methods to support interim batch release decisions. Some examples of the alternative test methods are growth-based detection methods using ATP bioluminescence or CO2 production and non-growth methods such as PCR-based methods.
How do regulators view alternative sterility testing methods for cell- and tissue-based products?
Regulatory agencies, including the FDA and EMA, acknowledge the need for faster sterility testing for cell- and tissue-based products. Regulatory acceptance is increasing, but companies must submit robust validation data to support the use of alternative sterility tests. The regulators require that alternative methods demonstrate performance comparable to or better than traditional compendial methods. A risk-based approach to sterility testing program may allow use of alternative methods in addition to compendial test methods to support interim release while the compendial method is performed in parallel.
How do you balance the need for sterility assurance with the preservation of cell viability and function?
This is one of the biggest challenges in sterility testing for cell- and tissue-based products. Overly aggressive sterility testing can deplete the product, while insufficient sterility testing may give insufficient data to guarantee product safety. One of the main strategies for balancing sterility assurance and product viability and function is performing testing on surrogate samples such as spent media instead of testing valuable therapeutic material itself. In addition, implementation of robust in-process testing at multiple time points, including the starting material, ensures early detection of contaminants and an increased chance of detection without consuming a significant amount of product at the end of the process. Designing a tailored, risk-based testing and release strategy ensures that regulatory and safety requirements are met without unnecessary product depletion.
 About The Experts:
About The Experts:
Anthony Thatcher is the senior director of manufacturing operations at Sumitomo Pharma America. He earned his bachelor’s degree at Gonzaga University and has an MBA from Rutgers University. He is also a member of the International Society for Pharmaceutical Engineering’s ATMP Community of Practice Steering Committee.
 Prethib Arumugam is the associate director of quality control for Sumitomo Pharma America. His career spans more than 15 years and includes the development of testing strategies for cell and gene therapies. He earned his bachelor’s degree in biotechnology at California State Polytechnic University, Pomona.
Prethib Arumugam is the associate director of quality control for Sumitomo Pharma America. His career spans more than 15 years and includes the development of testing strategies for cell and gene therapies. He earned his bachelor’s degree in biotechnology at California State Polytechnic University, Pomona.
